why the NT must delay opening its border to protect First Nations people
- Written by Claire Smith, Professor of Archaeology, College of Humanities, Arts and Social Sciences, Flinders University
The current string of COVID-19 outbreaks in Aboriginal communities in remote areas of the Northern Territory will only get worse if the NT government opens its borders on December 20, as planned.
The government should heed the call by John Paterson, CEO of the Aboriginal Medical Services Alliance NT (AMSANT), for the borders to remain closed until January and for a surge workforce to accelerate vaccinations and relieve exhausted medical staff.
AMSANT has also recommended 90% vaccination rates for Aboriginal people before the borders open. This is supported by key Aboriginal organisations, including the Northern Land Council.
The government’s current plan is that after the NT borders open, all arrivals will remain within the high vaccination zones of Greater Darwin, Katherine or Alice Springs for the first 14 days.
This plan has serious flaws. While double vaccination rates in Darwin are over 95%, in remote areas they average 72%.
If COVID-19 is transmitted within an urban centre, the locals might be protected by vaccinations. However, Aboriginal people visiting from remote areas are still vulnerable as they go to town to buy food or for medical attention or sport.
Aboriginal people are particularly vulnerable to COVID-19 due to high rates of chronic disease, overcrowded housing, high mobility and limited access to medical facilities.
Aboriginal perceptions of vaccines in remote areas
Since March 2020, we have been conducting research with the NT Aboriginal communities of Barunga, Beswick, Manyallaluk and Werenbun on cultural responses to COVID-19.
Most recently, our work has focused on people’s attitudes to vaccination. We’ve identified a mix of influences, including cultural, social, religious and physical access. As Jean Tiati, a resident in Barunga told us,
I’ve had my second vaccine. The first time I was really scared. One of my friends told me ‘When you get the vaccination, when the virus go in your body, it won’t make you sick, because it is too little’. After that, I said ‘Ok, I’ll go’.
Christianity in these communities exists alongside Aboriginal spiritual beliefs. Religion has been used to argue for and against vaccination. Tiati told us,
If people know Jesus, they can ask him for help. If you really trust Jesus, you can trust him to look after you if you have that vaccine. People that don’t want to get that vaccination they misinterpret the bible. They interpret that if they get that needle they’ll die. It’s the other way around for me: I get that needle and I’m safe.
Read more: Vaccinations need to reach 90% of First Nations adults and teens to protect vulnerable communities
Current outbreaks in communities
When COVID-19 first appeared in the NT, some Aboriginal people perceived it as a white man’s disease. However, recent outbreaks in Katherine have brought COVID-19 close to home.
A 78-year-old Aboriginal woman from Binjari was the first COVID-19 death in the Northern Territory earlier this month.
The high numbers of close contacts in these communities highlight the closeness of Aboriginal family networks. Lower vaccination rates can also make people feel vulnerable.
In Barunga, the double vaccination rate is 91%, but in Beswick/Wugularr, it’s just 64%. When COVID-19 was identified in wastewater a few days ago, one Beswick resident, Esther Bulumbara, said:
Everyone just got a shock. We didn’t know about it. We were frightened. My grandson rang me and say ‘Nanna, stay in the house. Nanna, you can’t walk around’.
While Beswick was subject to a three-day lockdown, Barunga residents just had to wear masks for 72 hours, due to the community’s higher vaccination rate.
Communities with medical clinics tend to have high vaccination rates, but there are still great disparities. At outstations, the rates are low. The Royal Flying Doctor Service is filling these gaps.
Mardi Steere is the executive general manager of the Royal Flying Doctor Service, which is working with Aboriginal community-controlled health organisations, such as Sunrise Health Services Aboriginal Corporation. Thus far, Steere told us, the Royal Flying Doctors have delivered 11,975 vaccine doses to 94 locations in South Australia and the NT.
Cultural barriers and enablers
Cultural attitudes to vaccination in Aboriginal communities can be different to those in mainstream society.
Vaccination rates in Aboriginal communities were initially slow due to government mistrust, intergenerational trauma and low literacy levels. Moreover, everyday racism has made Aboriginal people more cautious about the vaccines and could explain why the government didn’t prioritise the most vulnerable populations.
Principal influencers are family, Elders, traditional owners and custodians, and Aboriginal people employed at clinics. Over time, people who are unsure about vaccines become reassured as those they trust are safely vaccinated.
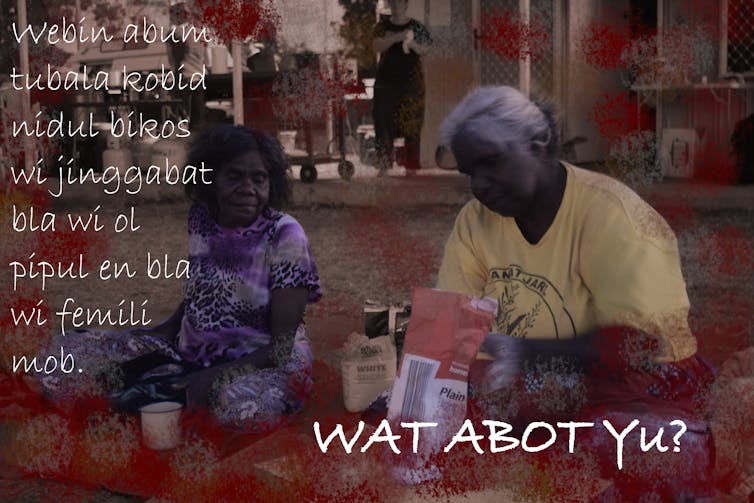
We’ve produced a series of posters in Kriol, personalised for each community. These expand on government information programs targeting Aboriginal people.
But misinformation has also contributed to vaccine hesitancy in many communities. Social media is influential, especially when the content is endorsed by a family member. As Galijan, a resident in Werenbun, told us:
There is a video of a man who created the vaccine. He is telling everyone to not get the vaccine. The man was talking in a school. Mum B. sent that video to me. That man said ‘if you don’t believe me, you’ll find out after you get the shot’.
We have found the most impactful information is communicated by Aboriginal people themselves through their own trusted networks and in media they use in their daily lives. Individuals and Aboriginal organisations also communicate urgent information through Facebook.
And people in quarantine have been using TikTok to reassure family members. As Rachael Kendino in Manyallaluk, told us:
They put it on TikTok. They do a little dance to tell other people that they are OK.
Aboriginal people encouraging a change of view
In the Katherine region, Aboriginal people who were once fearful are now seeking vaccinations. However, across the territory there are still many more people to vaccinate.
In the meantime, we need to delay opening the territory border. We need to listen to Elders, such as Narritj in Barunga:
They should have a roadblock from here to Gove. From the Arnhem Highway turnoff to Gove. Keep this area safe for old people from Barunga, right down to Gove. […] It’s very important. We don’t want any tourist mob coming in. We got to look after old people, so they can pass on the knowledge.
We are making progress but more needs to be done, such as:
more effective, targeted messaging about how COVID-19 is transmitted
more culturally safe ways of dealing with COVID-19, guided by traditional owners.
better ways to manage outbreaks in communities, such as mobile medical tents to minimise the trauma of people being locked up away from their Country and family when they need to quarantine. A facility in Katherine is also needed urgently.
Aboriginal people in remote areas have the answers. To protect these vulnerable communities, we need to listen to them.
Authors: Claire Smith, Professor of Archaeology, College of Humanities, Arts and Social Sciences, Flinders University





