Experts want Albanese to lead on indoor air quality as part of pandemic planning
- Written by Michelle Grattan, Professorial Fellow, University of Canberra
Last month, a delegation led by Brendan Crabb, head of the Burnet Institute, a prestigious medical research body, met Anthony Albanese in the prime minister’s parliament house office.
Its members, who included Lidia Morawska from Queensland University of Technology, a world-leading expert on air quality and health, also blitzed ministers and staffers. They were pitching for the federal government to spearhead a comprehensive policy on clean indoor air and for the issue to be put on the national cabinet’s agenda.
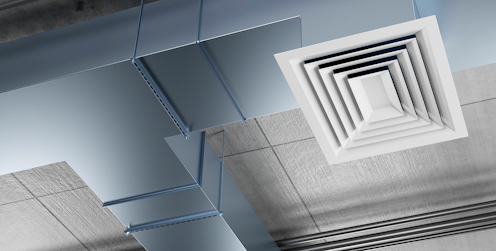
They pointed out to Albanese that indoor air is an outlier in our otherwise comprehensive public health framework. Despite people spending the majority of their time inside, indoor air quality is mostly unregulated, in contrast to the standards that apply to, for example, food and water.
There are multiple health and economic reasons to be concerned about this air quality but a major one is to limit the transmission of airborne diseases, such as COVID.
For many of us, COVID has become just a bad memory, despite its lasting and mixed legacies. For instance, without the pandemic, fewer people would now be working from home. More small businesses would be flourishing in our CBDs. Arguably, fewer children would be trying to catch up from inadequate schooling.
While the media have largely lost interest in COVID, and people are now rather blase about it, the disease is still taking a toll.
In 2023 there were about 4,600 deaths attributed to COVID, and almost certainly more in reality, given Australia that year had 8,400 “excess deaths” (defined as actual deaths above expected deaths).
Up to July this year there were 2,503 COVID deaths.
In nursing homes, whilst survival rates from COVID are much improved with vaccination and antivirals, as of September 19, there were 117 active outbreaks with 59 new outbreaks in that past week. There had been 900 deaths for the year so far.
Long COVID has become a serious issue, with varying respiratory, cardiac, cognitive and immunological symptoms. It is estimated between 200,000 and 900,000 people in Australia currently have long COVID.
The Albanese government is presently awaiting the report it commissioned into how the COVID pandemic was handled.
The inquiry has looked at the performance of the Morrison government, but its terms of reference didn’t include the states. That limits its usefulness, but there were politics involved, given high profile state Labor governments.
Not that the state and territory leaders of that time are around anymore (apart from the ACT’s Andrew Barr). Those faces that became so familiar from their daily news conference have disappeared into the never-never: Victoria’s Dan Andrews, Western Australia’s Mark McGowan, New South Wales’ Gladys Berejiklian, Queensland’s Annastacia Palaszczuk.
COVID variously made or tarnished leaders’ reputations. McGowan, in particular, reached stratospheric heights of popularity. Andrews deeply divided people.
In general, however, COVID boosted support for leaders and increased public trust in them and in government. In times of uncertainty, the public looked to known institutions and to authority figures. Since then, trust has eroded again.
Experts came into their own during the pandemic but then found themselves in the middle of the political bickering. In retrospect, some of them were wrong.
In the broad, especially in terms of the death rate and the economy, Australia navigated the crisis well. But drill down, and the story is more complex, as documented by two leading economists, Steven Hamilton (based in Washington and connected to the Australian National University) and Richard Holden (from UNSW).
In their just-published book, Australia’s Pandemic Exceptionalism, their bottom-line conclusion is that Australia was very impressive in its (vastly expensive) economic response but it was a mixed picture on the health side.
While Australia was quick out of the blocks in closing the national border and bringing in other measures, it fell down dramatically on two fronts. The Morrison government failed to order a wide variety of vaccines and it failed to buy enough Rapid Antigen Tests (RATs).
The “vaccine procurement strategy was an unmitigated disaster,” Hamilton and Holden write. This was not just “the greatest failure of the pandemic – it was arguably the greatest single public policy failure in Australian history”.
“We put all our vaccine eggs in just two baskets”, both of which failed to differing degrees. This was “a terrible risk to take. Pandemics are times for insurance, not gambling,” they write.
“And while our tax and statistical authorities marshalled their forces to operate much faster and more nimbly to serve the desperate needs of a government facing a once-in-a-century crisis, our medical regulatory complex repeatedly ignored international evidence and experience, and our political leaders capitulated to their advice. And then the prime minister told us that when it came to getting Australians vaccinated:‘it’s not a race’”.
The failure to order every vaccine on the horizon meant when production or supply problems arose for those that were hoped for or on order, the rollout was delayed.
After this bungle, “stunningly, we turned around and repeated these same mistakes all over again” by not obtaining and distributing freely massive numbers of RATs. In this failure, “our federal government showed the same lack of foresight, the same penny-wise but pound-foolish mindset that it had displayed in the vaccine rollout”.
The authors blame Scott Morrison, then-health minister Greg Hunt, then-chief medical officer Brendan Murphy, the Therapeutic Goods Administration (TGA), and the Australian Technical Advisory Group on Immunisation (ATAGI) for the health failures, which prolonged the lockdowns, cost lives and delayed reopening.
Urging better preparation for the next pandemic, Hamilton and Holden have a list of suggestions. They stress we need to ensure we have mRNA vaccine manufacturing capability (on which there is fairly good progress). We must get vaccine procurement “right from the start” regardless of cost. Huge quantities of RATs should be procured as soon as they become available, ready to be used immediately.
A complete overhaul of the medical-regulatory complex should be undertaken. As well, Australia should continue to invest in “economic infrastructure”. In the pandemic, the economic effort was facilitated by having a single touch payroll system. “The first obvious candidate for improvement is a real-time GST turnover reporting capability.”
Perhaps a comprehensive indoor clean air policy could be added to the infrastructure list.
The government’s review will have its own recommendations. Crabb and his colleagues hope they include attention to indoor air quality, following advice from the Chief Scientist and the National Science and Technology Council.
Members of the delegation say they received an attentive hearing from the PM.
Anna-Maria Arabia, chief executive of the Australian Academy of Science, and a member of the delegation, says Albanese “understood that improving indoor air quality is a cornerstone requirement to preparing for future pandemics and [he] was attuned to the practical implications of having good indoor air quality systems, including schools and workplaces being able to stay open and functional, reduce absenteeism and boost productivity”.
What’s needed beyond awareness, however, is timely policy action. Pandemics don’t give much notice of their arrival.
Authors: Michelle Grattan, Professorial Fellow, University of Canberra





