We studied 217 tropical cyclones globally to see how people died. Our findings might surprise you
- Written by Wenzhong Huang, Postdoctoral Research Fellow, School of Public Health and Preventive Medicine, Monash University
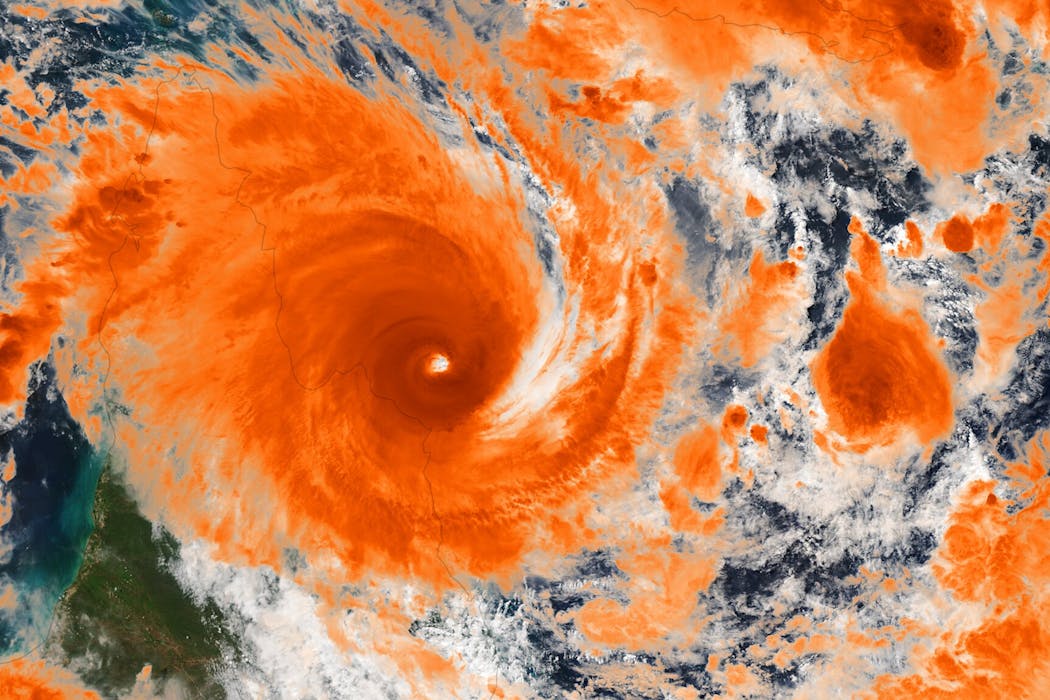
Tropical cyclones – also known as hurricanes, typhoons or storms, depending on their location and intensity – are among the world’s most destructive and costly climate disasters.
Their direct physical impacts, such as injuries and drowning, are well known.
But what about the wider health effects in the days and weeks after a cyclone? As health systems are disrupted and other issues arise, what happens next?
We analysed 14.8 million deaths in 1,356 communities around the world that had 217 tropical cyclones between them.
In our paper published today in the BMJ, we show what, and who, we should be focusing on if we are to prevent more people dying after these devastating events.
Why we’re interested in this
Each year, tropical cylones affect more than 20 million people and rack up around US$51.5 billion in damage globally.
In recent years, these cyclones have been getting stronger and lasting longer. They are expected to become more intense as our climate warms.
As well as wanting to know the wider health effects of tropical cyclones, we wanted to find out how these differ between countries and territories.
For instance, how do the wider health effects differ in countries such as Australia, which usually see fewer cyclones, compared to cyclone “hot zones”, such as those in East and Southeast Asia, or the eastern coast of the United States?
Understanding these differences is important given the shifting behaviour of tropical cyclones in a changing climate. This may include a greater risk in historically less-affected regions.
What we did
Our research team collected data from 1,356 communities across Australia, Brazil, Canada, South Korea, Mexico, New Zealand, the Philippines, Taiwan and Thailand between 2000 and 2019.
We combined death records with modelling of wind and rainfall patterns for each cyclone. This allowed us to assess relationships of cyclone windspeed and rainfall with the risk of dying from various causes afterwards. We also accounted for seasonal variations in mortality, and other factors.
What we found and what could explain it
The results were striking. Risks of dying from various causes consistently increased after a tropical cyclone. Generally, the risk peaked within the first two weeks of the cyclone, followed by a rapid decline.
Over the first two weeks, the largest increases were seen in deaths from kidney disease (up 92%) and injuries (up 21%) per cyclone-day in the first week. The more cyclone-days, the greater the cumulative risk.
We found more modest increases for deaths from diabetes (15%), neuropsychiatric disorders (such as epilepsy) (12%), infectious diseases (11%), gut diseases (6%), respiratory diseases (4%), cardiovascular diseases (2%) and cancer (2%).
So why is this happening? A combination of disrupted essential health care, limited access to medications, and increased physical and psychological stress likely explain our findings.
For example, power outages, flooding, or transportation disruptions caused by cyclones might stop the regular dialysis for people with kidney disease, creating life-threatening complications.
Rain may be even more deadly
We also found that rainfall from tropical cyclones is more strongly associated with deaths than wind, especially for cardiovascular, respiratory and infectious diseases.
This may be because the hazards associated with heavy rainfall, such as flooding and water contamination, can be more deadly than the direct impacts of strong winds, particularly for certain diseases.
So early warning systems for tropical cyclones may need to place greater emphasis on cyclone-related rainfall as well as windspeed.
Poorer countries were worse off
A similar study in 2022 focused on deaths after cyclones in the US. But when we studied more countries, we found higher risks of cyclone-related deaths.
We also found people living in poorer communities are substantially more likely to die from various causes after tropical cyclones.
These health gaps appeared to be most pronounced for kidney, infectious and gut diseases, as well as diabetes, reflecting existing health inequities.
Notably, countries and communities that rarely experienced cyclones but were now exposed to them were at greater risk of cyclone-related deaths. This may reflect a lack of effective response systems in areas with historically fewer cyclones.
The findings also highlight that many areas in the world that have had few cyclones historically, including Australia and higher-latitude regions, cannot afford to be complacent. With climate change, cyclone tracks and intensity are shifting, and these places may be especially vulnerable.
Where to next?
To reduce the health impacts of tropical cyclones, health departments’ disaster planning must look beyond immediate injuries and infrastructure damage. They need to prepare for a surge in medical needs across a range of diseases.
Emergency management agencies need to invest in poorer communities to reduce the persistent and significant health inequities they face during disasters such as cyclones.
Meteorological departments should also integrate more health data and epidemiological evidence into cyclone early warning and management systems to better protect vulnerable populations.
Authors: Wenzhong Huang, Postdoctoral Research Fellow, School of Public Health and Preventive Medicine, Monash University





